Safer Patients, Stronger Systems: Turning Competence into Measurable Value
What if the most powerful safety device isn’t a device at all?
If safety were a product, competence would be the operating system. Treat it like an add-on and improvements stall. Make it measurable, and the whole system starts to move.
On a medical ward, a 30-second fall-risk check and a quick room tweak avert a near-miss. Nothing heroic – just everyday excellence. The question is: how do we scale it?
Competence isn’t a checklist—it’s infrastructure
When clinical judgment, communication, teamwork, and continuous improvement are visible in data, they become a shared operating system. Teams see the same picture, align faster, and move evidence into daily practice—strengthening safety, quality, and system sustainability.
Our testbed: pairing people + tech for fall prevention
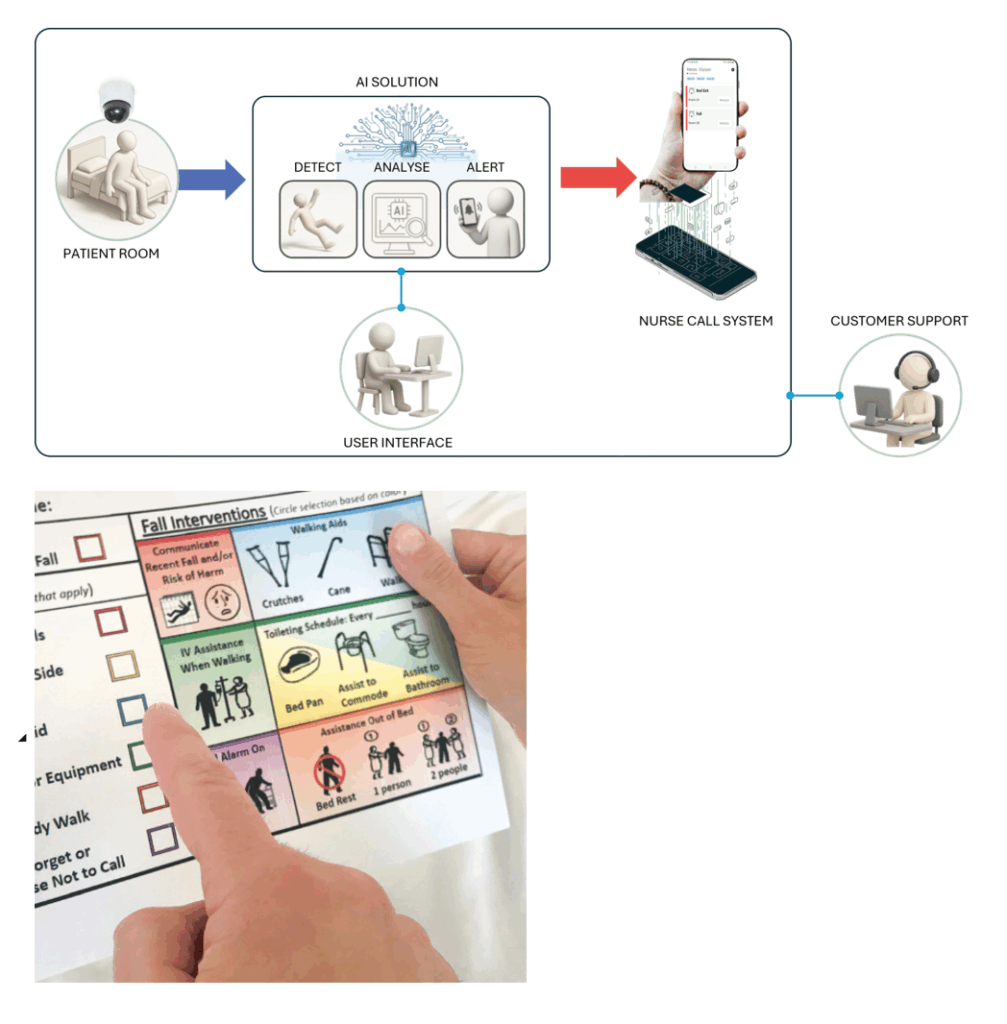
We’re evaluating two complementary tools:
- Fall TIPS — structured bedside planning with patients and families. https://www.ahrq.gov/patient-safety/settings/hospital/fall-tips/index.htm
- Vision-based monitoring — real-time alerts for unsafe movement. https://versovision.com
We track a full chain of evidence so value shows up end-to-end:
Clinical (falls & harm/1,000 pt-days), Operational (length of stay, alarm load), Economic (costs avoided vs. program costs), Staff experience (confidence, adoption), and Resource footprint (materials & energy per bed-day).
Lesson: technology works when competence and routines carry it – audits, feedback loops, and staffing patterns that make the safer way the easier way. Outcomes: fewer harms, shorter stays, freed resources, and frontline ownership.
Three moves to close the knowing–doing gap
- Make competence visible. Shared measures turn “skills” into navigational data – strengths, gaps, next steps.
- Link practice to outcomes, costs, and footprint. One value story: fewer injuries, shorter stays, better use of staff time and materials.
- Build a learning culture. Normalize questions, small tests of change, and learning from near-misses
In short
Treat competence as infrastructure; pair it with the right tools and routines; make the value story visible-clinical, operational, financial, and resource use. That’s how nursing delivers safer care today and a more resilient system tomorrow.

Visiting Researcher,
Department of Nursing Science,
Faculty of Health Sciences,
University of Eastern Finland